There is a problem with the recently approved Alzheimer’s drug, Aduhelm. It can remove some of the amyloid that forms brain plaques that are hallmarks of the disease. But most of the drug is wasted because it hits an obstacle, the blood-brain barrier, that protects the brain from toxins and infections but also prevents many drugs from entering.
Researchers wondered if they could improve that grim result by trying something different: they would open the blood-brain barrier for a short time while they delivered the drug. Their experimental method was to use highly focused pulses of ultrasound along with tiny gas bubbles to pry the barrier open without destroying it.
The investigators, at the Rockefeller Neuroscience Institute at West Virginia University, reported their results last week in The New England Journal of Medicine. When the barrier was opened, 32 percent more plaque was dissolved, said Dr. Ali Rezai, a neurosurgeon at the institute, who led the study. The group did not measure the amount of antibody getting in — that would require radioactively labeling the drug — but in animal studies opening the barrier allowed 5 to 8 times more antibody to enter the brain, Dr. Rezai said.
The early-stage experiment, which was only tried in three patients with mild Alzheimer’s, was funded by the university and the Harry T. Mangurian, Jr. Foundation.
It was a preliminary safety study — the first stage in research — and not designed to measure clinical outcomes.
But when the results were presented at a recent meeting, “our mouths opened,” said Dr. Michael Weiner, an Alzheimer’s researcher at the University of California in San Francisco who was not involved in the study.
Researchers said it was an innovative but difficult approach to a problem that Dr. Walter Koroshetz, director of the National Institute of Neurological Disorders and Stroke, deemed one of the most challenging in treating brain diseases: How do you get drugs into the brain?
Antibodies like the Alzheimer’s drug aducanumab, which the company Biogen sells as Aduhelm, are extremely expensive; the listed price of Aduhelm is $28,000 a year. One reason for the high price, Dr. Koroshetz said, is that only 1 percent of the antibodies injected into the bloodstream slip past the blood-brain barrier.
Finding a safe way to open that barrier took more than a decade, though. Investigators understood how the barrier worked, but opening it without causing any damage meant keeping it open for just a short time, because of its role in protecting the brain. It is a fragile part of circulatory system and not what many people envision, based on its name.
“A lot of people think of it as a thing that is wrapped around the head,” like a turban for the brain, said Dr. Alexandra Golby, a professor of neurosurgery and radiology at Harvard Medical School.
Instead, the barrier is at the ends of several major blood vessels that supply the brain. As they enter the head, the vessels branch and divide until, at their tips, they form narrow capillaries with extremely tight walls. This barrier keeps large molecules out and allows small molecules like glucose and oxygen to get in.
The challenge was to pry those walls open without ripping the capillaries apart.
The solution turned out to have two components. First, patients are injected with tiny microbubbles of perfluorocarbon gas. The bubbles range in size from 1.1 to 3.3 microns (a micron is about 0.000039 inch.) Then, pulses of low frequency ultrasound are focused on the area of the brain to be treated. The ultrasound pulses set up waves in the fluid in blood vessels; the microbubbles rapidly expand and contract with the waves. This pries open the vessels without damaging them, providing entree into the brain.
Microbubbles, Dr. Golby said, are used routinely in ultrasound imaging studies of the heart and liver because they light up, revealing blood flow. They are filtered out of the body by the kidneys and liver.
“They have a twenty-year track record of being safe,” she said.
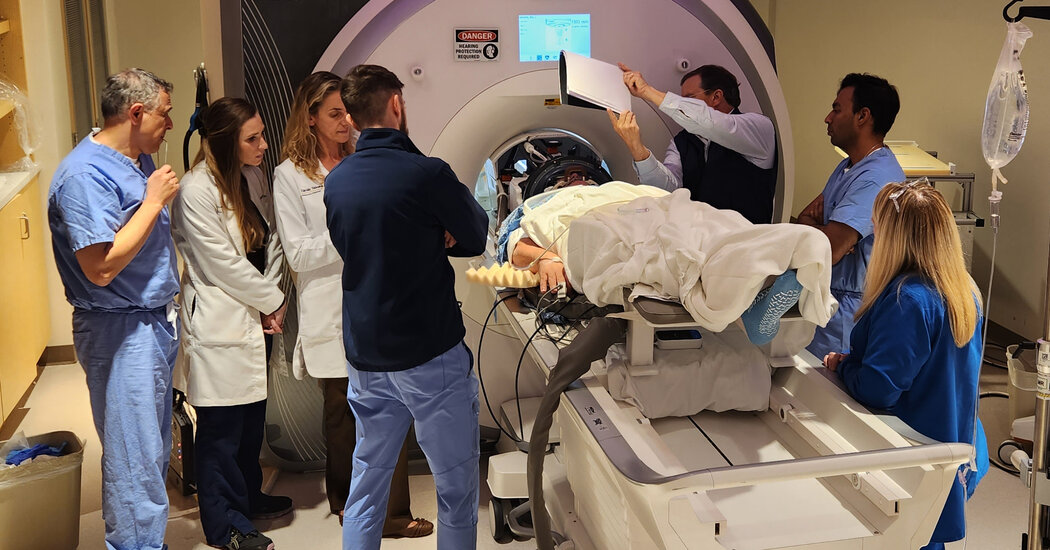
For the experiment described in the new paper, researchers used ultrasound on one side of the brain but not the other, for comparison, then performed brain scans to check the results.
While the focused ultrasound approach proved successful as an experiment, all was not rosy. The device was designed to deliver ultrasound to a small targeted area, but in cases of Alzheimer’s, amyloid-containing plaque is all over the brain.
“If you want to get amyloid out of the brain, you want to go in with a paint brush, not a pencil,” Dr. Koroshetz said.
The researchers deliberately hit brain areas involved with memory and reasoning, but it remains to be seen whether the treatment improves outcomes. That will require a larger study.
The Alzheimer’s study is just one of several that involve opening the barrier to deliver drugs to patients with a variety of brain diseases.
All are in early stages and all, so far, show that the method works; drugs that were blocked get in.
One group, led by Dr. Nir Lipsman, a neurosurgeon at the Sunnybrook Research Institute of the University of Toronto and his colleagues, opened the barrier to deliver a chemotherapy drug to the brains of four breast cancer patients whose cancer had spread to the brain. The concentration of the drug, trastuzumab, increased fourfold, they reported.
That work was funded by the Focused Ultrasound Foundation and sponsored by Insightec, which manufactures the ultrasound device used.
Dr. Lipsman and his colleagues have now treated seven breast cancer patients, and are expanding the study. They also are conducting preliminary studies in a variety of brain diseases, including cancer, Parkinson’s, and A.L.S.
Dr. Golby, at Harvard Medical School, and her colleagues have used the method to treat patients with glioblastoma, a deadly brain cancer.
One of the few chemotherapeutic agents that can get into the brain is temozolomide. But even it is mostly blocked; only 20 percent gets past the blood-brain barrier.
So Dr. Golby’s medical center and several others got permission from the Food and Drug Administration to do a clinical trial, using focused ultrasound with microbubbles to deliver more of the chemotherapy. It was funded by Insightec.
The patients did well, but the purpose of the study, which has not yet been published, was to assess the safety of the technique, not its efficacy, she said.
“I would love to see a trial of a drug that doesn’t normally get into the brain,” Dr. Golby said. There are many drugs that look great in laboratory studies but, she said, “totally fail,” because they are blocked by the blood-brain barrier.
For now, though, questions remain — like where in the brain to target the therapies.
But, said Dr. Jon Stoessl, a Parkinson’s expert and professor of neurology at the University of British Columbia, the method “does away with the problem that has historically been an issue for anyone treating central nervous system disorders.”
Kullervo Hynynen, vice president for research and innovation at Sunnybrook Research Institute in Toronto, is hopeful.
“If this works and is safe, it opens doors to a completely new way of treating brains,” he said.